Highlights
How can lean, healthy children still exist? If American infants are born into a world where they will eat fast food, travel by car, and spend their free time on TV and video games, why aren’t all children obese and diabetic? If the answer is genes, why has the search for “genes that make you fat” failed so completely?1 Simple questions often lead to better science, and the quest to answer these simple questions led to a novel theory of childhood disease based on the idea that there are evolutionary consequences to how a mother spends her day.
Maternal Effects
In evolutionary biology, the term “maternal effects” describes how a mother’s characteristics, such as her body size and behavior, affect the health and survival of her offspring, independent of her genes. Until recently, the term was limited to insects and other non-human animals, but in January of this year, I published a paper that posits maternal effects in humans have snowballed from one generation to the next, leading to the twin epidemics of childhood obesity and type II diabetes.
The theory is simple: for good or for ill, mothers’ health behaviors—think diet, exercise, drug and alcohol use, and so on—before, during, and after pregnancy determine the body mass, metabolism, and health behaviors of their kids, and their daughters in turn determine the body mass, metabolism, and health behaviors of future generations. When a pregnant woman is physically active, the increased energy demands of activity redirect calories and nutrients to her muscles and away from her developing child. This competition between the mother’s muscles and the developing child’s fat cells produces leaner, healthier kids who grow up to be leaner, healthier parents.
When mothers are inactive, this competition does not occur, thereby producing infants predisposed to increased birth weight, obesity, and metabolic disease. These children may also be more inactive as adults as a result of observing and imitating their mothers’ (and fathers’) inactivity. I think that today’s racial and socioeconomic disparities in childhood health are the result of differences in health behaviors (e.g., TV viewing, exercise) and consequent body size being passed down progressively from one generation to the next. These effects arise primarily through mothers because it is their behavior during pregnancy that “programs” the child’s metabolism in the womb.
Obesity and Type II Diabetes
Over the past three decades, the prevalence of obesity has more than doubled in children and quadrupled in adolescents. Yet not all children are overweight or obese, and there are significant disparities across and within demographic groups. For example, non-Hispanic black children are significantly more likely to be obese than non-Hispanic white children,2 and the prevalence of morbid obesity (BMI ≥ 40 kg/m2) in black children is more than three times that of whites.3 Importantly, children from single-parent households are significantly more likely to be obese than children from traditional (married) two-biological parent households, independent of race.4,5
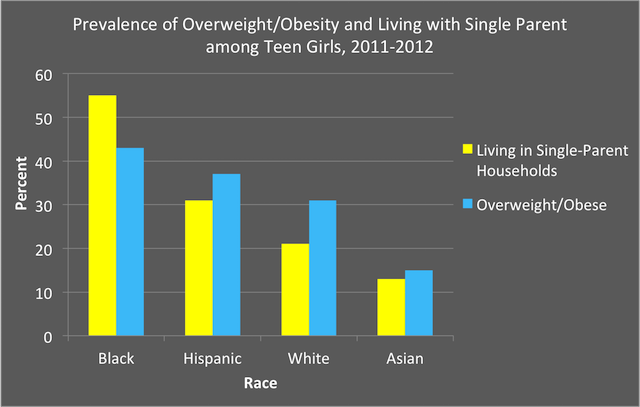
Over the past few decades, trends and rates of obesity6 and type II diabetes7 parallel those of single-parent households.8 The figure below depicts the percentage of 12- to 19-year-old girls of each race who were overweight/obese and living in single-parent households in 2011-2012.2,9,10 This theory suggests the disparity in obesity and metabolic diseases between children raised in traditional intact families and those raised in single-parent households11-13 is driven primarily by progressive differences in maternal health behaviors over multiple generations (i.e., accumulating ‘maternal effects’).
Pregnancy and Metabolic Health
Physical activity is an absolute requirement for metabolic health,14,15 and for most of human history, the amount of physical effort required by daily life kept both mother and her unborn child healthy. Yet beginning in the mid-twentieth century, the physical activity necessitated by motherhood and daily life decreased exponentially due to labor- and time-saving devices like cars, washing machines, and dishwashers. From the 1960s to 2010, the amount of physical effort mothers expended at work and in the home decreased by 1200 to 1500 calories per week.16,17 In fact, by the mid-1990s, women were spending more time watching TV than on all forms of physical activity, such as housework and exercise, combined.16,18 By the mid-2000s, pregnant women reported spending more than 60 percent of their waking hours in sedentary behavior (e.g., TV/computer use).19
Yet there were significant differences in these health behaviors based on family structure, and single mothers quickly became the most inactive segment of the U.S. population.16,20,21 While inactivity has dire effects on all adults’ health, low levels of physical activity and/or high levels of sedentary behavior during pregnancy are extremely detrimental to both mother and developing fetus. Inactive pregnant women face increased risks of gestational diabetes, pre-eclampsia, preterm birth, and excessive gestational weight gain,22 which can lead to excessive fetal growth, obstructed labor, and maternal mortality.23,24 As noted earlier, inactivity alters a mother’s energy metabolism during pregnancy, which negatively and permanently increases the risks of obesity and type II diabetes in her children.24 Over time, these risks will be substantially amplified as children growing up with inactive mothers are more likely to be inactive and obese, and to suffer from metabolic disease as adults,24 thereby perpetuating an intergenerational cycle of obesity and disease.
Absentee-Father & Single-Mother Effects
The prevalence of both single-parent households and child/adolescent obesity have more than tripled since the early 1970s,25,26 and there is a strong relationship between single-mother households and overweight/obesity in children (especially girls) that is independent of family income.4,5 This suggests that the negative health effects of single-mother households are due to something other than financial hardships. Raising kids always takes a lot of time, and in single-parent families, there is only one adult to meet those burdens. Thus single mothers spend less time caring for and playing with their children than married, co-resident parents.27
Moreover, to cope with time demands, single mothers often eliminate their own physical activity while using TV as a babysitter for children,28 which has significant impacts on health and development. A struggling single mother’s future children will be impacted by her altered body mass and metabolism, and her current children will exhibit lower levels of physical activity and higher levels of sedentary behavior than other kids,27-30 placing them at an elevated risk of obesity, metabolic diseases, and impaired cognitive development.31-34
When a child is active, the calories he or she eats are used to build muscle, bone, and metabolic health. Conversely, when a child is sedentary, more of those calories go to building fat mass, increasing the risks of metabolic diseases such as type II diabetes.24,35 When inactive, obese female children reach puberty, their fat mass can increase exponentially and their physical activity will decrease as a consequence of weight gain. When these girls become mothers, their obesity and inactivity will be progressively propagated to the next generation, leading to an ever-worsening cycle of obesity and inactivity. With about half of black children, versus roughly a quarter of Hispanic children and a fifth of white children, residing in single-parent households, the theory of maternal effects also helps explain why black women are the most inactive, obese, and therefore the most metabolically compromised portion of the U.S. population.36-39
Conclusion
My theory suggests that the proximate cause of the increasing disparity in childhood obesity and metabolic diseases is the increased frequency of negative maternal health behaviors, which result not just from environmental changes but also from the time demands imposed by absentee fathers. These negative health behaviors and the consequent obesity are passed down from mothers to children to grandchildren. If we as a nation are to break this cycle of inactivity, obesity, and metabolic disease, we first need to address the cultural and societal influences that drive women to become single, overburdened mothers and cause men to be absent from the lives of their children.
Dr. Edward Archer, Ph.D., is an obesity theorist and computational physiologist with the Nutritional Obesity Research Center at the University of Alabama, Birmingham. He has authored numerous scientific publications that have been profiled in the New York Times, L.A. Times, ABC News with Diane Sawyer, Huffington Post, and many other media outlets.
References
1. Veerman JL. On the futility of screening for genes that make you fat. PLoS Med. 2011;8(11):e1001114.
2. Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA. 2014;311(8):806-814.
3. Skelton JA, Cook SR, Auinger P, Klein JD, Barlow SE. Prevalence and Trends of Severe Obesity among US Children and Adolescents. Academic pediatrics. 2009;9(5):322-329.
4. Huffman FG, Kanikireddy S, Patel M. Parenthood—A Contributing Factor to Childhood Obesity. International Journal of Environmental Research and Public Health. 2010;7(7):2800-2810.
5. Augustine JM, Kimbro RT. Family Structure and Obesity Among U.S. Children. Journal of Applied Research on Children: Informing Policy for Children at Risk. 2013;4(1):5.
6. Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999-2010. JAMA. 2014;307(5):483-490.
7. Dabelea D, Mayer-Davis EJ, Saydah S, et al. Prevalence of type 1 and type 2 diabetes among children and adolescents from 2001 to 2009. Jama. 2014;311(17):1778-1786.
8. Martin JA, Hamilton BE, Ventura SJ, Osterman MJK, Wilson E, Mathews T. Births: Final Data for 2010. National Vital Statistics Reports. 2012;61(1).
9. Vespa J, Lewis JM, Kreider RM. America’s Families and Living Arrangements: 2012; Current Population Reports, P20-570. Washington, DC: U.S. Census Bureau; 2013.
10. Caprio S, Daniels SR, Drewnowski A, et al. Influence of Race, Ethnicity, and Culture on Childhood Obesity: Implications for Prevention and Treatment: A consensus statement of Shaping America's Health and the Obesity Society. Diabetes Care. 2008;31(11):2211-2221.
11. Schwartz JE, Friedman HS, Tucker JS, Tomlinson-Keasey C, Wingard DL, Criqui MH. Sociodemographic and psychosocial factors in childhood as predictors of adult mortality. American Journal of Public Health. 1995;85(9):1237-1245.
12. Hayward MD, Gorman BK. The Long Arm of Childhood: The Influence of Early-Life Social Conditions on Men's Mortality. Demography. 2004;41(1):87-107.
13. Wood RG, Goesling B, Avellar S. The Effects of Marriage on Health: A Synthesis of Recent Research Evidence. Washington, DC: U.S. Department of Health and Human Services; 2007.
14. Blair SN. Physical inactivity: the biggest public health problem of the 21st century. Br J Sports Med. 2009;43(1):1-2.
15. LaMonte MJ, Blair SN, Church TS. Physical activity and diabetes prevention. J Appl Physiol. 2005;99(3):1205-1213.
16. Archer E, Lavie CJ, McDonald SM, et al. Maternal Inactivity: 45-Year Trends in Mothers’ Use of Time. Mayo Clinic Proceedings. 2013;88(12):1368-1377.
17. Church TS, Thomas DM, Tudor-Locke C, et al. Trends over 5 decades in U.S. occupation-related physical activity and their associations with obesity. PLoS One. 2011;6(5):e19657.
18. Archer E, Shook RP, Thomas DM, et al. 45-Year Trends in Women's Use of Time and Household Management Energy Expenditure. PLoS One. 2013;8(2):e56620.
19. Evenson KR, Wen F. Prevalence and correlates of objectively measured physical activity and sedentary behavior among US pregnant women. Prev Med. 2011;53(1-2):39-43.
20. Dlugonski D, Motl RW. Marital status and motherhood: implications for physical activity. Women & health. 2013;53(2):203-215.
21. Robinson JP, Godbey G. Time for life: The surprising ways Americans use their time. 2nd ed. University Park, PA: Pennysylvania State University Press; 1999.
22. Evenson KR, Chasan-Taber L, Symons Downs D, Pearce EE. Review of Self-reported Physical Activity Assessments for Pregnancy: Summary of the Evidence for Validity and Reliability. Paediatr Perinat Epidemiol. 2012;26(5):479-494.
23. MSDoH. Infant and Maternal Mortality Surveillance. 2015.
24. Archer E. The Childhood Obesity Epidemic as a Result of Nongenetic Evolution: The Maternal Resources Hypothesis. Mayo Clinic Proceedings. 2015;90(1):77-92.
25. USCB. America’s Families and Living Arrangements: 2003 Current Population Reports. United States Census Bureau 2004.
26. Ogden CL, Fryar CD, Carroll MD, Flegal KM. Mean body weight, height, and body mass index, United States 1960-2002. Adv Data. 2004(347):1-17.
27. Kendig SM, Bianchi SM. Single, Cohabitating, and Married Mothers’ Time With Children. Journal of Marriage and Family. 2008;70(5):1228-1240.
28. Taveras EM, Hohman KH, Price S, Gortmaker SL, Sonneville K. Televisions in the bedrooms of racial/ethnic minority children: how did they get there and how do we get them out? Clinical pediatrics. 2009;48(7):715-719.
29. Lindquist CH, Reynolds KD, Goran MI. Sociocultural determinants of physical activity among children. Prev Med. 1999;29(4):305-312.
30. Bowman SA, Harris EW. Agricultural Research Service, US Department of Agriculture; Research Brief: Food security, dietary choices, and television-viewing status of preschool-aged children living in single-parent or two-parent households. . Fam. Econ. Nutr. Rev. 2003;15:29–34.
31. Gortmaker SL, Must A, Sobol AM, Peterson K, Colditz GA, Dietz WH. Television viewing as a cause of increasing obesity among children in the United States, 1986-1990. Arch Pediatr Adolesc Med. 1996;150(4):356-362.
32. Carson V, Janssen I. Volume, patterns, and types of sedentary behavior and cardio-metabolic health in children and adolescents: a cross-sectional study. BMC Public Health. 2011;11:274.
33. Tremblay MS, LeBlanc AG, Kho ME, et al. Systematic review of sedentary behaviour and health indicators in school-aged children and youth. Int J Behav Nutr Phys Act. 2011;8:98.
34. Christakis DA, Zimmerman FJ, DiGiuseppe DL, McCarty CA. Early Television Exposure and Subsequent Attentional Problems in Children. Pediatrics. 2004;113(4):708-713.
35. Church T. Exercise in obesity, metabolic syndrome, and diabetes. Prog Cardiovasc Dis. 2011;53(6):412-418.
36. Andersen RE, Crespo CJ, Bartlett SJ, Cheskin LJ, Pratt M. Relationship of physical activity and television watching with body weight and level of fatness among children: Results from the third national health and nutrition examination survey. JAMA. 1998;279(12):938-942.
37. Sisson SB, Broyles ST. Social-ecological correlates of excessive TV viewing: difference by race and sex. J Phys Act Health. 2012;9(3):449-455.
38. Getahun D, Strickland D, Lawrence JM, Fassett MJ, Koebnick C, Jacobsen SJ. Racial and ethnic disparities in the trends in primary cesarean delivery based on indications. Am J Obstet Gynecol. 2009;201(4):422 e421-427.
39. Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity among adults: United States, 2011-2012. NCHS Data Brief. 2013(131):1-8.














