Highlights
Editor's Note: The following research brief, originally published on March 11, 2020, is our third most popular post of the year.
The novel coronavirus, now dubbed COVID-19, has sickened over 113,000 people around the world and killed over 4,000 (at the time this report was written). Normal people from Italy, to Iran, to China, to Korea, and even now in the United States have rushed to stores to buy food, hand sanitizer, masks—all in preparation for what is now taken for granted by many, that containment of COVID-19 will fail. At this point, most public health experts concede that COVID-19 will infect a very large number of people, and as a result, may cause a considerable number of deaths. One epidemiologist claimed that COVID could infect between 40-70% of the world’s adult population. Given that COVID is estimated to be fatal in somewhere between 0.5% and 5% of cases, this projection would mean anywhere from 15 to 200 million deaths around the world, and somewhere between 500,000 and 10 million deaths in the United States.
In all likelihood, actual death tolls will be far lower. Vaccines are already in development, treatment options are improving, and governments are aggressively responding to the threat, imposing quarantines and other measures to reduce the spread of the disease. But still, a major pandemic is likely.
But when we think about the effect of pandemics on demography, it’s important to look at not only deaths but also births. Illness, quarantine, and death can all have a major impact on conception, pregnancy, and birth. In this research brief, I will lay out what we know about how epidemic diseases, and governmental responses to them, influence birth rates, and what that may tell us about how COVID-19 will shape the ongoing decline in global birth rates.
COVID is very likely to reduce births in the near term, and perhaps by a quite considerable amount. But after the epidemic has passed, fertility in countries other than China is likely to rebound, especially if death tolls have been significant or if governments take action to replace lost wages, like expanding paid sick leave or extending unemployment insurance benefits. But thanks to China’s uniquely anti-natalist policy stance, no large fertility rebound is expected there.
Disasters Impact Fertility
The relationship between high-mortality events and future fertility patterns is well-established in the academic literature. Previous academic literature has shown that high-mortality events as diverse as famines, earthquakes, heatwaves, and disease all have very predictable effects on reducing births nine months later. The figure below presents estimates from “death spike” events from the academic paper linked above, as well as Hurricane Maria, Hurricane Katrina, and the 2015 Ebola outbreaks in Liberia, Sierra Leone, and Guinea.
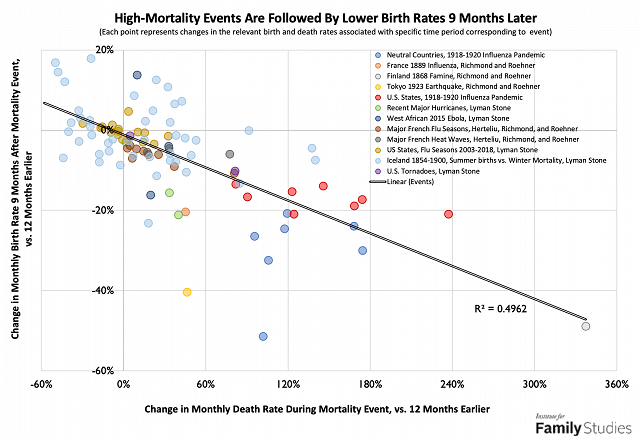
As can be seen, deaths and births are closely related. Events that cause a large increase in deaths tend to cause a large decrease in births nine months later. This relationship holds up for influenza outbreaks in 1889, 1918, France since 1950, and the U.S. since 2003. It holds up across three major hurricanes in the U.S. and two large hurricane outbreaks. It fits the case of Ebola mortality in West Africa, an earthquake in Japan, three French heatwaves, the last large famine in Finland in 1868, as well as the entire distribution of winter mortality and summer fertility in Iceland in the 19thcentury. Across numerous contexts, lots of death leads to fewer conceptions, and thus fewer births nine months later.
But the effect is far from consistent. Aside from normal historic variation from many causes, events that kill a very large number of people do cause fewer births, but not by as much as might be expected. In other words, a disease that kills 5% of the population won’t reduce births by 5 times as much as a disease that kills 1% of the population. This nonlinear effect is hypothesized to be due to what the researchers cited above call “collateral survivors,” that is, people who suffer disruption in their life due to a disaster but do not actually die.
Identifying this disruption is a challenge. “Collateral survivors” could be people whose home is destroyed by a hurricane, people who survive a painful illness, or people who lose a spouse to disease. But they could also by people who lose wages from work or are simply traumatized by fear during a crisis. Any large mortality event will produce a considerable number of collateral survivors.
But after this loss, fertility tends to rebound. Figure 2 below presents the change in local birth rates in areas hit by various crises. Some are high-mortality events like the 1918 influenza epidemic or Hurricane Maria. But others caused comparatively few deaths: monthly deaths in Hong Kong barely budged during the 2003 SARS outbreak, and Zika is very mild for infected adults.
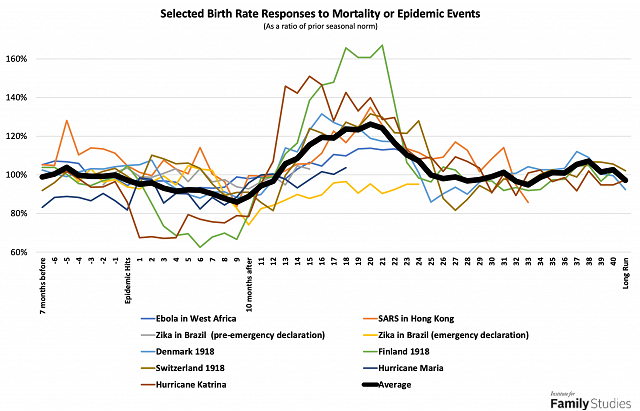
As can be seen, starting around 10 or 11 months after an epidemic, birth rates begin to recover.
Academic research confirms the presence of such rebounds. In Sweden, Norway, Taiwan, Japan, India, and the United States, the 1918 influenza epidemic reduced births just after the epidemic, but then increased births in the subsequent 1-5 years. In the long run, effects varied: in Sweden and Norway, marriage markets were disrupted, leading to a durable decline in births thanks to more people being widowed, and fewer married. But in India, long-run fertility rose as a reduced population led to more agricultural land for each family. Strikingly, similar patterns have been observed even in aboriginal Melanesians experiencing their first contact with Western diseases.
It should be noted that while “collateral survivors” mostly determine reduced birth rates in the 9 months after an epidemic, death rates may have an important role to play in the recovery: the loss of children, family members, and friends can provoke "mortality-replacement" or "recuperative fertility." For example, after the 2004 Indian Ocean tsunami, women in communities that experienced tsunami deaths saw their fertility rise sharply relative to other women. The main effect identified here arises, not from the immediate family of victims, but from those in the community around them. The fear and trauma of loss motivated higher fertility, an effect identified in many disasters of various kinds.
This fear and trauma, this sense of existential insecurity, has been found to motivate higher fertility in other cases as well. Researchers have found that both the Cuban Missile Crisis and the Oklahoma City Bombing had fertility impacts, and some have even suggested that 9/11 had a similar effect.
Thus, for the first few years after a major crisis, fertility trends are fairly predictable: births decline and then rise. The long-run trend, as well as the scale of an effect, can be much more difficult to determine. Specific factors related to a crisis such as whether it alters marriage markets, attitudes towards nonmarital childbearing, and government responses can all have large effects. But the most important factor is simply the scale of a disaster: disasters impacting more people have larger effects on both mortality and fertility. While deaths attract a great deal of attention, the number of impacted people who don’t die might be even more important. A disease that disrupts economic activity and marital behaviors, and which infects or scares a very large number of people, may have a very large effect indeed, even if it does not kill very many.
Who Is Impacted?
All epidemic diseases can be described using two basic statistics: the case-fatality rate (CFR), meaning the share of people who get the disease who will end up dying of it, and the rate of spread of the disease, formally called “R0” or “r-naught,” also known as the "reproduction rate," which is a number showing how many people an infected person is likely to infect. For every disease discussed here, CFR and R0 statistics will be provided to help compare to COVID. COVID has a CFR of between 0.5% and 5%, as noted above, and an R0 of between 1 and 3.
It's natural to start any analysis of COVID’s possible effects with other epidemics, and indeed to start at the last truly massive global pandemic: the “Spanish flu” of 1918-1920. The Spanish flu1 killed somewhere between 17 and 100 million people or about 1 to 6% of the world's population. Based on estimates of the infected share of the population, implied CFR estimates for Spanish flu range from 2% to 20%. Meanwhile, academic research suggests that Spanish flu’s R0 value was between 2 and 4 in the general population: so each infected person spread the disease to between 2 and 4 other people. However, COVID’s best-estimated R0 comes from a study of a confined population (passengers on the Diamond Princess cruise ship), whereas Spanish Flu’s R0 in confined populations (as shown in the previously linked paper) was about 2.6 to 10.6. COVID is probably both considerably less contagious than Spanish flu, and likely somewhat less lethal, and thus has a lower potential for a massive epidemic. So whatever effect Spanish flu had on birth rates, COVID should have a similar but smaller effect.2
The R0 value, in particular, is important, because it may be a reasonable indication of how many collateral survivors there will be: people who get sick (or fear getting sick) but don’t die. Because COVID is very infectious, but not extremely lethal, there will likely be a large number of collateral survivors, suggesting that births in the immediate wake of a COVID outbreak should fall considerably. Note in the second graph above, for example, that Ebola caused only a very small decline in births in west Africa, likely because it killed about 40% of those infected, and ultimately spread to less than 50,000 people: collateral survivorship was fairly low thanks to extremely high mortality.
Estimating the Effect of COVID
In the short run, some predictions can be ventured. If 10% of the population of America is infected, and they experience a 0.5% mortality rate, then a very simple model would suggest that this would have virtually no impact on fertility whatsoever. If, on the other hand, 30% of the population is infected, and mortality is near the World Health Organization’s current estimates of 3.5%, effects could be larger: births 9 months from now could fall by half.
Estimating birth recoveries is even more uncertain, but the academic papers cited above suggest that mortality replacement fertility ranges from 0.25 births added for each epidemic casualty (or birth loss) in the 1-5 years after an epidemic, to as high as 2 births added. Using the infection spread and fatality rate estimates as above, and the mortality-replacement estimates mentioned, estimates of medium-term fertility recuperation are very wide: COVID could boost births over four years after the epidemic runs its course by anywhere from 0.3% to 40%.
Obviously, these estimates are next to useless: the range is far too large. The extent of mortality replacement is extremely variable across different contexts, and COVID’s likely scale remains uncertain as well. This makes it very hard to narrow the range of forecasts. But the figure below presents some different scenarios on how birth rates could respond to different epidemic profiles.
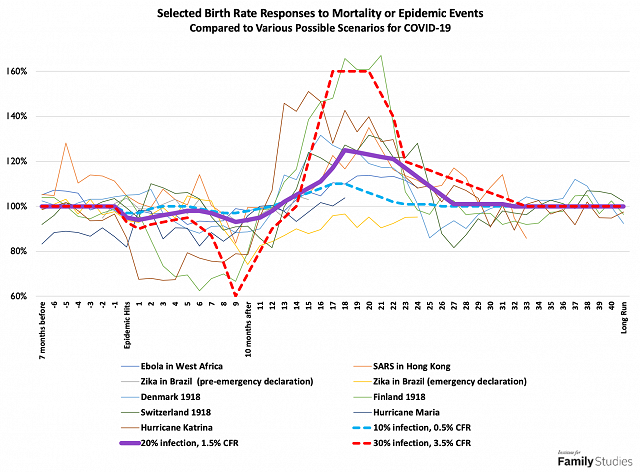
There is an additional wrinkle in forecasting these effects, however. Public and governmental responses are even harder to predict than epidemiological outcomes and may be even more decisive. As the second graph in this post showed, the effect of Zika on Brazilian birth rates was modest: but the effect of the Brazilian government’s public health advisories about Zika was very large. Political and social conditions can impact the relationship between epidemics and fertility. For example, if social disruptions lead to power outages, that might cause a bit of a baby boom 9 months later. But mere work stoppages probably don’t impact fertility. In the United States, mild storm advisories have been shown to lead to increases in birth rates 9 months later (probably due to couples being cloistered together), while serious storms tend to reduce birth rates (probably due to economic damages).
I have been unable to identify any study of the fertility impact of social distancing and quarantine measures. However, it’s possible that such measures could be similar to storm advisories in effect, leading to small increases in birth rates. On the other hand, social distancing measures are probably bad for the economy and could lead to income losses for some households, and thus could reduce birth rates.
If COVID infections and deaths rise to epidemic levels (that is, rise to hundreds of thousands of cases in America), then any positive quarantine effect would almost certainly be mitigated by mortality and collateral survivorship, as well as economic effects. But if Americans take proactive measures to stay home together more and avoid going out, and in so doing also succeed in preventing COVID from spreading widely, and if policymakers take measures to keep the economy humming, then U.S. birth rates could actually rise slightly in the next year as a result of COVID.
The key factors to watch are:
- How many people live in households where someone was infected, or in communities that had significant levels of local transmission (collateral survivorship)?
- Is mortality from all causes rising, or are COVID deaths being offset by fewer deaths from other causes like influenza (mortality replacement)?
- To the extent mortality from COVID occurs, is it large enough among reproductive-age people to meaningfully alter the marital status distribution of the population? Are weddings being postponed to a significant degree (marriage market effects)?
- Are people actually staying home with their significant others more frequently as a result of quarantine or social distancing measures (possible quarantine baby bumps)?
- Has COVID led to significant, negative economic disruptions, especially boosting unemployment (economic effects)?
Right now, in America, very few people have experienced any kind of collateral survivorship, and there have been only a few confirmed deaths. Certainly, there have been no documentable marriage market effects yet, and social distancing has also not occurred to a very appreciable degree, although this is changing rapidly. Some negative economic effects may have begun, but they are very mild. Thus, if COVID gets no worse than it is now, then no birth rate impact would be expected.
On the other hand, in Wuhan, virtually the entire population can be considered a “collateral survivor,” and mortality has been significant enough that it seems unlikely that all COVID deaths would have been due to influenza or other respiratory deaths (COVID probably increased Wuhan’s mortality rate in January and February by about 2 to 7%, by my calculations). Mortality in Wuhan has been heavily concentrated among older people, however, so probably has not impacted marriage markets. That said, China’s continuing anti-natal restrictions and norms, and stigmas against non-marital childbearing, limit the potential for mortality-replacement fertility after COVID has passed. The entire population of Wuhan has been quarantined, which should produce some baby bump, except that China’s economic output has collapsed, suggesting that economic losses are large. Furthermore, anecdotal evidence suggests that quarantines may have led to more divorces than babies. Thus, in Wuhan, we can expect a considerable drop in births over the next 10 months with only very modest potential for mortality-replacement-style recoveries later on.
Every country is different, and so different countries will have different experiences. As more information becomes available, possible fertility impacts will become clearer. For now, we should all be washing our hands frequently, enforcing good hygiene for everyone in our household and place of business, and making plans for how to protect our communities in the event of a major outbreak.
Lyman Stone is a Research Fellow at the Institute for Family Studies, Chief Information Officer of the population research firm Demographic Intelligence, and an Adjunct Fellow at the American Enterprise Institute. He was formerly a market forecaster for the U.S. Department of Agriculture.
1. Note that the designation “Spanish flu” is unfair to Spain; the disease did not originate in Spain, but either in a French military hospital, southwest China or possibly even Kansas or Boston
2. Spanish flu isn’t the only major influenza outbreak. The “Asian Flu” of 1957, “Hong Kong flu” of 1968, “Russian flu” of 1977, and H1N1 (which originated in Mexico) in 2009 have all led to large shares of the global population being infected, and many people dying: but their estimated CFRs are far below Spanish flu, under 0.3% in all cases. However, even these diseases probably did impact fertility, as shown in the first figure. But these influenza pandemics were not only less lethal but also less contagious, than the 1918 pandemic, with R0 values between 1.2 and 1.9. Ebola’s R0 is around two, while Zika’s R0 depends entirely on the presence of nearby mosquitoes, thus ranging between zero and 10. Stomach bugs like norovirus range from R0 values of one to eight.














